Erectile dysfunction (ED), a condition affecting millions globally, is often misunderstood. While many factors can contribute to its onset, the intricate relationship between low testosterone and ED warrants a closer examination. This exploration aims to demystify this connection, presenting a factual account of how these two conditions interact and what the implications are for diagnosis and treatment.
Testosterone, a primary male sex hormone, plays a pivotal role in a man’s overall health and well-being, extending far beyond its association with masculinity. Its influence on sexual function is multifaceted, acting as a conductor for various physiological processes essential for a healthy sex life. Understanding these fundamental roles is crucial before delving into its link with ED.
The Basics of Testosterone Production and Function
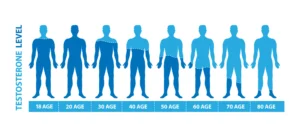
Produced primarily in the testes and in smaller amounts by the adrenal glands, testosterone levels naturally fluctuate throughout a man’s life. Production typically peaks in adolescence and early adulthood, gradually declining with age. This gradual decline, known as andropause or the “male menopause,” can, in some individuals, lead to levels that impact their physical and psychological health. Beyond its direct sexual effects, testosterone is instrumental in maintaining muscle mass, bone density, red blood cell production, mood regulation, and energy levels. Its presence is, therefore, a cornerstone of male vitality.
Testosterone’s Reach: Libido and Desire
One of the most well-established roles of testosterone is its impact on libido, or sex drive. It acts as a powerful catalyst for sexual desire and arousal. When testosterone levels are adequate, men typically experience normal levels of interest in sexual activity. Conversely, a significant drop in testosterone can lead to a diminished libido, where the desire for sex wanes. This reduction in desire can be a significant precursor to, or concurrent symptom of, ED, as a lack of sexual interest can make achieving or maintaining an erection less likely or even a secondary concern.
The Indirect Influence on Erections
While testosterone is essential for libido, its direct role in the physical mechanism of erection is less pronounced than commonly believed. Erections are primarily a vascular and neurological event, heavily reliant on nitric oxide production and smooth muscle relaxation within the penile tissue. However, testosterone plays an indirect but important supporting role. It helps maintain the health and responsiveness of the penile tissues, including the smooth muscle and blood vessels, over the long term. Without sufficient testosterone, these tissues may become less pliable and less capable of responding robustly to the stimuli that trigger an erection. Think of testosterone as the essential maintenance crew for the machinery of erection; while it might not be the switch that turns it on, its absence can lead to the machinery becoming rusty and less functional over time.
The Prevalent Link: Low Testosterone in Men with ED
The observation that a significant proportion of men presenting with erectile dysfunction also exhibit low testosterone levels is a recurring theme in clinical practice and research. This statistical association has led many to assume a direct causal link, but the reality is more nuanced, a complex tapestry rather than a simple thread.
Statistical Prevalence: A Significant Overlap
Studies have consistently shown a high prevalence of hypogonadism, or low testosterone, among men diagnosed with ED. Depending on the study and the definition of low testosterone used (often an arbitrary threshold like <400 ng/dL or <300 ng/dL), nearly half of men with ED may have testosterone levels below the normal range. This statistic is compelling and undeniable; it highlights that these two conditions often walk hand in hand. However, it is crucial to recognize that correlation does not equate to causation. The presence of low testosterone in a large percentage of ED patients does not, in itself, prove that low testosterone is the sole or even primary driver of their erectile issues.
Beyond the Numbers: Understanding the Contributing Factors
The observed overlap is likely due to a confluence of shared risk factors that contribute to both low testosterone and ED. Conditions such as obesity, type 2 diabetes, metabolic syndrome, cardiovascular disease, and chronic inflammation are known to negatively impact both gonadal function (leading to lower testosterone production) and vascular health (impairing the erectile process). Therefore, when these underlying conditions are present, they can simultaneously suppress testosterone and directly compromise the physical ability to achieve and maintain an erection. In essence, these shared culprits are often the architects of both problems.
Navigating the Complexity: Low Testosterone is Not Always the Primary Culprit
While the prevalence of low testosterone in ED patients is undeniable, it is a vital distinction to make that it is rarely the sole or initiating cause of erectile dysfunction for the majority of men. The intricate mechanisms of erection involve a delicate interplay of vascular, neurological, hormonal, and psychological factors, and low testosterone, while a contributing element, often plays a supporting or exacerbating role rather than leading the charge.
Vascular Issues: The Silent Engine of ED
The primary driver of ED for most men, particularly as they age, is impaired blood flow to the penis. This vascular component is often the first and most significant hurdle. Conditions like atherosclerosis (hardening of the arteries), hypertension (high blood pressure), and diabetes can damage the delicate blood vessels in the penis, restricting the blood flow necessary for an erection. These conditions can compromise the smooth muscle function and endothelial nitric oxide production, which are the workhorses of the erectile process. It is like trying to fill a garden hose with a kink in it; no matter how much pressure is applied, the water flow will be insufficient.
The Psychological Dimension: The Mind-Body Connection
The mind plays a profound role in sexual function. Performance anxiety, stress, depression, relationship issues, and guilt can all create significant psychological barriers to achieving an erection. These psychological stressors can trigger the body’s “fight or flight” response, which diverts blood away from the extremities, including the penis, making an erection difficult or impossible. In such cases, even with optimal testosterone levels and healthy vascularity, psychological factors can act as a potent inhibitor.
Medications and Lifestyle: Unseen Saboteurs
A wide range of prescription medications, including those for blood pressure, antidepressants, and even some pain relievers, can have ED as a side effect. Lifestyle choices also play a substantial role. Smoking damages blood vessels, excessive alcohol consumption can impair nerve function and hormonal balance, and a sedentary lifestyle contributes to weight gain and poor cardiovascular health. These factors can individually or collectively undermine the complex systems required for a healthy erection.
The Therapeutic Landscape: Testosterone Replacement Therapy (TRT) and ED
When low testosterone is confirmed to be a significant factor, Testosterone Replacement Therapy (TRT) emerges as a potential treatment option. However, understanding its precise impact on ED is crucial; it is not a universal panacea and its benefits are often concentrated in specific areas of sexual function.

Boosting Libido and Mood: Reliable Benefits
One of the most consistent and reliably observed benefits of TRT is its positive effect on libido and overall mood. For men experiencing a significantly reduced sex drive due to hypogonadism, TRT can often reignite their desire for intimacy. This improvement in sex drive can be quite pronounced and is a primary indication for therapy. Furthermore, adequate testosterone levels are linked to better energy, reduced fatigue, and improved mood regulation. Many men on TRT report feeling more energetic and less prone to depressive symptoms, which indirectly can contribute to a more positive outlook on sexual activity.
The Nuance of Erectile Function Improvement
The effect of TRT on the physical aspect of erectile function is, by contrast, often more nuanced and less dramatic. While some men with low testosterone may see an improvement in their ability to achieve and maintain erections with TRT alone, this is not universally the case. TRT’s contribution to erections is largely indirect, by improving the health and responsiveness of penile tissues over time, rather than directly facilitating the immediate vascular event of erection. For many, TRT may improve their baseline erectile capacity, making them more responsive to other treatments, or it might be insufficient on its own to overcome existing vascular or neurological impediments. It is like ensuring the car’s engine is running smoothly; it makes it more likely to perform well, but it doesn’t fix a flat tire.
Synergy with Other Treatments: A Combined Approach
For a significant proportion of men with ED and low testosterone, TRT is most effective when used in conjunction with other ED treatments, particularly phosphodiesterase-5 (PDE-5) inhibitors such as sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra). These medications directly address the vascular component of ED by increasing blood flow to the penis. When combined, TRT can improve the underlying hormonal environment and tissue health, while PDE-5 inhibitors provide the immediate vascular support. This synergistic approach often yields the most comprehensive improvements in erectile function. The combination allows for both a healthier foundation and a more potent immediate response.
Long-Term Efficacy and Considerations
The long-term efficacy of TRT for ED can vary. While improvements in libido and mood may be sustained, the impact on erectile function can sometimes diminish or plateau over time, especially if underlying vascular or neurological issues are progressive. Furthermore, TRT is a lifelong commitment with potential side effects that require ongoing monitoring, including an increased risk of blood clots, prostate issues, and sleep apnea. Therefore, a thorough discussion with a healthcare professional is essential to weigh the benefits against the risks and to establish realistic expectations regarding long-term outcomes.
When to Consider Screening: Identifying the Role of Low Testosterone
The decision to screen for low testosterone in men experiencing erectile dysfunction is a clinically informed one, guided by a constellation of symptoms and patient circumstances. It is not a universal recommendation for all men with ED, but rather a strategic diagnostic step in specific scenarios.
The Red Flags for Low Testosterone
Several indicators suggest that low testosterone might be a significant contributor to a man’s ED. Beyond the physical act of experiencing erectile difficulties, men may report a noticeable decline in their libido or sexual interest. Persistent fatigue, a decrease in muscle mass or strength, and a tendency towards a more somber or depressed mood can also be associated with hypogonadism. If a man presents with ED alongside these other symptoms, it raises the suspicion that low testosterone is playing a role in his overall health, including his sexual function.
Patients Unresponsive to Standard Treatments
A particularly strong indication for testosterone screening involves men whose ED has not adequately responded to first-line treatments, such as PDE-5 inhibitors. If Viagra or Cialis, when taken correctly and in appropriate dosages, fail to produce satisfactory results, it suggests that the underlying cause of the ED might not be solely vascular or that there are additional contributing factors at play. In such cases, low testosterone becomes a more likely suspect, and testing can help to uncover this potential obstacle to successful treatment. It’s a bit like trying a common key that doesn’t work; it’s time to explore alternative locks.
Comprehensive Health Assessment
Screening for low testosterone is often integrated into a broader health assessment for men with ED. This comprehensive approach acknowledges that ED is frequently a harbinger of underlying health issues. By testing testosterone levels, a physician can gain valuable insights into a patient’s endocrine health and identify potential imbalances. Even if low testosterone is not the primary cause of ED, its treatment can lead to improvements in other health parameters, such as a reduction in abdominal fat and an improved metabolic profile, which can, in turn, positively influence erectile function. It is about treating the whole person, not just the symptom.
Conclusion: A Collaborative Approach to Sexual Health
The link between low testosterone and erectile dysfunction is a complex interplay, not a simple cause-and-effect relationship. While low testosterone can significantly impact libido and contribute to ED, it is rarely the sole perpetrator. Vascular issues, psychological factors, medications, and lifestyle choices often play more dominant roles in the genesis of erectile dysfunction.
For men experiencing ED, a thorough evaluation by a healthcare professional is paramount. This assessment should include a comprehensive history, physical examination, and appropriate diagnostic testing, which may include testosterone levels, especially if standard treatments are ineffective or if other symptoms of hypogonadism are present.
If low testosterone is confirmed, Testosterone Replacement Therapy (TRT) can be a valuable component of treatment, particularly for improving libido and mood, and for enhancing the overall responsiveness to other ED therapies. However, it is crucial to have realistic expectations, as TRT alone may not fully resolve erectile dysfunction.
Ultimately, addressing ED effectively requires a collaborative approach between patient and physician, one that considers all potential contributing factors and tailors the treatment plan to the individual’s unique needs. By understanding the nuanced relationship between testosterone and erectile function, men can make informed decisions about their sexual health and work towards achieving greater satisfaction and well-being.


